Bariatric Surgery – An Overview

Marla Evans hated diabetes and the lifestyle changes good glycemic control demanded of her. She described herself as a “denial diabetic” after her initial Type 2 diagnosis in 2004, when she was 49. Six daily medications slowed but didn’t stop her diabetes, because diet changes and exercise weren’t part of her life. By 2007, her weight of 220 was at least 70 pounds too high. With a Body Mass Index of 35 and an A1c above 9, she was on a dangerous road destined to end in a hospital emergency room. All this she knew, but the behavior changes required seemed out of reach. Like many people with diabetes, she felt trapped in a struggle she could not win. “I knew I was slowly killing myself,” Evans recalled, “but I couldn’t make myself do enough to prevent it.”
As Thanksgiving 2012 approaches, Evans said she weighs 155 pounds and “feels great.” A gastric bypass performed in 2007 by Dr. Philip Schauer as part of the STAMPEDE program at Cleveland Clinic changed her life. STAMPEDE, or “Surgical Therapy And Medications Potentially Eradicate Diabetes Efficiently,” delivered Evans more than promised. She lost 65 pounds, her diabetes is gone, and so are her medications. She is a poster child for the benefits of bariatric surgery, not just for weight loss, but also for its benefits in reversing Type 2 diabetes. Indeed, Cleveland Clinic and other institutions around the country are starting to describe these procedures as “diabetes surgery” rather than “weight-loss surgery.”
Evans’ experience also shows how a dramatic intervention like bariatric surgery can produce major behavior changes that far exceed those required, in theory, to lose weight and control her diabetes the old fashioned way. Of course, the kicker here is that her diabetes doesn’t need to be controlled, because it no longer exists. The dietary and lifestyle trade-offs following bariatric surgery are as significant, perhaps even more extremely challenging, than those required for good diabetes control. But somehow, the hospital admission, the surgical process itself, and most of all, the discharge that sends a majority of patients home with no diabetes medications on board and none required, seems to make it all worthwhile. It’s the kind of dramatic intervention that helps convince people that things are different now, and so they must behave differently too.
Shrinking the Stomach
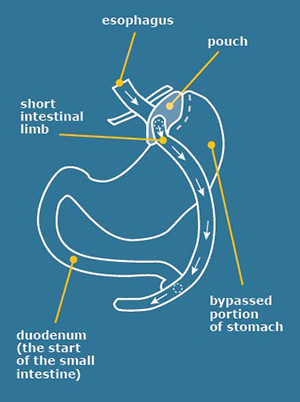
There are four different procedures under the bariatric surgery umbrella, of which gastric bypass is the most frequently performed. The operation entails two steps. Step one makes the stomach smaller. A surgeon uses staples to divide the stomach into a small upper section and a larger bottom section. The top section of the stomach (called the pouch) is where the food one eats now goes. A normal stomach, when full, can be as large as an NFL football. The pouch is about the size of a walnut or a golf ball, and holds only three ounces, or less, of food. The second step is the bypass, which connects the new, small stomach to the small intestine (the jejunum) through a tiny hole in the pouch. The food one eats will now travel from the pouch into this new opening to reach the small intestine. As a result, the body will absorb fewer calories, and of course, require a lot less eating to make one feel full.

Today, most bariatric procedures are done laparoscopically. The surgery costs between $20,000 and $30,000, and post-operative hospital stays are normally one or two days. Fifteen years ago, bariatric surgeries were relatively rare and quite risky, entailing long hospital stays and weeks of convalescence, not to mention many complications. As Dr. Schauer noted, today’s bariatric procedures are about as risky as gall bladder or hysterectomy surgeries, which are common and carry few serious risks.

Who’s Eligible?
Criteria vary from one insurance carrier to another, but in general, a candidate for surgery needs to have a Body Mass Index (BMI) of 35 or more (about 60 pounds overweight) and at least one complication of obesity, such as diabetes, to qualify initially. Almost all insurers require a long process before approval, including submitting medical records that prove the subject has tried and failed, under supervision, to lose weight through diet and exercise; that the patient has received counseling about emotions and eating habits; and that his or her A1c score has remained above the maximum normal percentage of seven for a long period of time, despite faithful use of medications, including insulin.
Because she was the very first patient who participated in the STAMPEDE program, Evans avoided most of these screenings and the required nine months to a year they entail. Her surgery was paid for by the research grants covering the trial. But she did have to consider a lengthy list of caveats before consenting to surgery. The bypass changed her daily life in many ways.
Learning How to Eat Again
After a gastric bypass, the patient doesn’t just have a much smaller stomach. He or she also uses less of the small intestine — because part of it is bypassed — to absorb and distribute the calories and nutrients in food. The combination compels a number of changes in eating behavior and daily routine.
The first requirement is a high-protein diet. Evans must consume 60 to 80 grams of protein a day. There are about 7 grams of protein in an ounce of meat, and the new stomach only holds 2 to 3 ounces. So meeting her protein target requires eating between 4 and 6 protein-rich small meals a day — similar to the multiple small meals recommended for many people with diabetes. Consuming protein bars and drinks helps Evans to meet her daily goals, but she cautioned that careful label reading is required to make sure she gets the most bang for her protein buck.
For reasons that aren’t clearly understood, gastric bypass surgery also changes the way the “gut” communicates with the brain. Appetite is reduced, taste buds change, and so does food tolerance. “Breakfast was my favorite meal,” Evans said, “but I can’t eat eggs or yogurt anymore without getting sick.” She must now add ice cream, another favorite, to the list. Drinking during the two hours around meal time is also off limits. That’s because the liquid can fill the smaller stomach without providing needed protein. When does Evans eat vegetables and starches? “When I have room,” she said. The protein is more important than a “balanced” diet. Another imperative part of the daily routine entails consuming vitamins and mineral supplements.
It’s a complex and demanding routine, but it’s a regimen Evans embraces because of how good she feels, not to mention the way she looks on a size 10 dress rather than the size 20 she used to wear. “I believe that by following all the [post-surgery] rules, I’ve avoided all complications,” Evans said.
Where Are All The Patients?
The success of Evans’ diabetes cure through gastric bypass is no fluke. Up to 80 percent of gastric bypass or other bariatric procedures designed to produce weight loss had the same successful results in people with Type 2 diabetes over the past five years. Major studies published this year in prestigious medical publications such as the New England Journal of Medicine and Journal of the American Medical Association support not only the relative safety of the procedure but also its role in diabetes remission and dramatic cost savings over the lives of the patients treated.
Bariatric surgery, is “the underperformed surgery you should be getting,” according to the popular and credible Dr. Oz.
But bariatric surgery, like the operation performed on Evans, is “the underperformed surgery you should be getting,” according to the popular and credible Dr. Oz. The key word in the quote is “underperformed.” Oz believes that less than one percent of those who qualify for the procedure receive it. There will be about 200,000 bariatric procedures performed this year in the U.S., quite an increase from 10 or 15 years ago. Nevertheless, this is still a tiny percentage of the millions of people with Type 1 or Type 2 diabetes who are obese or morbidly obese according to BMI measures. Why aren’t thousands of candidates lined up at the doors of the 450 hospitals around the U.S. where they can get the surgeries? As you might expect, there are a number of answers to that question, including inertia in the medical world, reluctance of insurers to pay, and the failure to measure or understand wellness return-on-care investment.
Change Comes Slowly
The majority of diabetes cases — particularly Type 2 — is diagnosed by primary care physicians in family practice, and that’s where care remains. Having learned one way to treat people with diabetes, it’s hard to adopt another. (This applies to endocrinologists, too.) This is especially true when the doctor-patient relationship is strained, as is often the case with Type 2 diabetics, who are famously prone to being non-compliant with medical advice.
 Insurers bear part of the responsibility, too. As pointed out above, even when insurance coverage is available, daunting — and for some, an impossible amount of — paperwork is required.
Insurers bear part of the responsibility, too. As pointed out above, even when insurance coverage is available, daunting — and for some, an impossible amount of — paperwork is required.
Meanwhile, a shortsighted concern with the up-front costs prevails over a focus on the long-term return on investment and excellent medical outcomes that the surgeries would provide. In the last two years, at least three major studies comparing significant numbers of bariatric surgery recipients with control populations of diabetics who have similar weight and A1c characteristics concluded that the cost of surgery was fully recovered within 24 to 26 months. Post-surgery, expenses for diabetes supplies and medications completely disappear in many patients. Considering that the estimated lifetime cost of medications and supplies is 175,000 to $200,000 per diabetic diagnosed at age 50 and up, it is clear that the $30,000 surgery is eminently cost-effective.
Even when the procedures don’t cure diabetes, they often pay off in substantial savings. For Type 1 patients who received the surgery, medication costs dropped by an average of 46% over the study periods.
Is This a Cop-out?
Are these bariatric surgery recipients taking the easy way out? If you’re a Type 1 in good control, able to enjoy 3 meals a day plus ice cream thanks to your pump and CGM, you might prefer that to the rigorous routines that are required after gastric bypass surgery. But for many with diabetes whose present condition and future complications loom over the health care landscape like a gigantic black cloud, it may be that bariatric surgery’s time has come. They might get nauseous from eating too much ice cream, but that is a small price to pay for heading off heart attacks, strokes, blindness, and amputations.





