Making Insulin Easier
Insulin Patch to provide simpler insulin therapy that automatically responds to your blood glucose for better diabetes management
![Researchers were able to preload enough insulin into the coin-sized adhesive microneedle patches to enable clinical use. [Image courtesy of UCLA]](https://www.type2nation.com/wp-content/uploads/2020/03/Compressed-Patch.jpeg)
Living with diabetes can leave you feeling like a human pincushion on a daily basis. Injections, finger-pricks, CGM sensors, and infusion sites all require piercing your skin with very sharp objects.
A new development from a research team led by UCLA is hoping to offer people with diabetes an insulin patch containing “microneedles” that will today’s syringes and pen-needles a thing of the past!
Led by Zhen Gu, a bioengineering professor at UCLA, the team has created an insulin patch that is about the size of a small coin plus the surrounding adhesive that holds it in place.
Pre-filled with Insulin
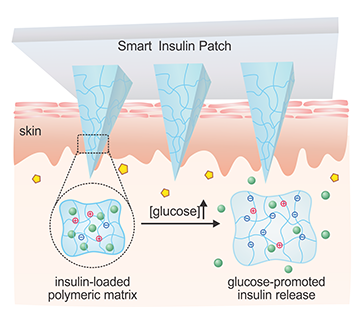
The patch is about the size of a quarter and is pre-filled with insulin. Microneedles on the inside of the patch deliver insulin through the person’s subcutaneous flesh by just penetrating the outermost layer of the skin.
Today’s syringes, pens, or pumps also deliver insulin into subcutaneous flesh, but they penetrate much deeper whereas these microneedles go unnoticed by the person wearing the patch.
Created with a molding and UV light-curing process, the patches are able to maintain the safety and potency of insulin for more than two months when kept at room temperature.
“The microneedle patch provides such a convenient, painless way to apply a glucose-responsive insulin delivery system to people with diabetes,” Gu said.
Medical technologists have tried many times to create an insulin patch, but Gu’s technology is different because it doesn’t rely on a chemical reaction to stimulate the release of insulin and is less likely to irritate a person’s skin.
The patch’s adhesive technology is also unique. It’s non-degradable and completely removable and it does not interfere with the delivery of insulin. Gu, however, is keeping that aspect of his technology to himself, declining to describe in greater detail how he designed the adhesive.
It is even possible to “personalize” the patches to adjust the amount of insulin released, theoretically matching each patient’s precise insulin needs.
For example, one patch could serve as a long-acting or “background” insulin, and another patch could be applied for every meal. The patches could vary in size based on what you planned to eat. These options are still largely in development, but it’s clear that Gu and his team understand that one size does not fit all when it comes to insulin needs.
Glucose-responsive Technology
The best part of this system is that the patch actually releases insulin based on the person’s glucose levels, which should lower the risk and frequency of low blood sugars.
“There’s a large amount of insulin inside (the patch), and we’re making the whole needle matrix glucose-responsive,” explained Gu in an interview with Medical Design & Outsourcing.
When the glucose in a person’s interstitial fluids (the fluid in your tissue) rises above normal levels, the “phenylboronic acid units” cause the needles to swell and release insulin.
The patches have been tested in controlled studies on “diabetic minipigs.” The glucose-responsive technology was able to maintain normal blood sugar levels for more than 20 hours.
During the study, the patches also proved to lower high blood sugar levels within 1 to 2 hours. Traditional delivery of insulin via syringe would lower high blood sugar levels within 2 to 3 hours.
Evolution of the Insulin Patch
Gu’s initial interest in helping patients with diabetes started with his grandmother who passed away from complications related to type 2 diabetes.
I understand their pain, and I understand their inconvenience,” Gu explains.
He began working on the development of an insulin patch during his postdoctoral fellowship at the Massachusetts Institute of Technology Lab with well-known entrepreneur Robert Langer.
Langer and Gu worked together originally with a grant he’d received for diabetes-related research.
Gu eventually served as a Biomedical Engineering Professor at the University of North Carolina at Chapel Hill, and at North Carolina State University.
At NCSU, Gu began working with Dr. John Buse, who was already highly regarded by the American Diabetes Association for his work on hundreds of clinical studies, epidemiologic analyses, and other projects.
Development Funding
A startup company funding the research and development of Gu’s insulin patch is his own company, Zenomics. It acquired a $5.8 million dollar investment from the biomedical device company MicroPort Scientific Corporation in 2017.
Langer now serves on the Zenomics’ board, continuing to support Gu’s work.
“It has been a pleasure to see the terrific progress by [Gu] and his team,” said Langer. “It could someday lead to new ways of treating diabetes and other diseases.”
John Buse gives a great deal of credit to Gu for the insulin patch.
“He’s the brains of the operation,” said Buse. “I just try to keep him focused on how to develop this into something that works in persons.”
Practical Hopes
Buse hopes the patch provides, at the very least, a backup method for delivering insulin for those who currently rely on insulin pumps, but a significant number of people with type 1 diabetes do not use insulin pumps as they are costly and require 24-hour wear.
“The genius of [the patch] is if you could have something that was relative unobtrusive,” said Buse, “…which fundamentally is like a Band-Aid, and the patch would release insulin in response to glucose levels. You would basically solve the diabetes problem in many ways.”
The technology still has a long way to go as it approaches human trials and continues to develop patches that may need to be replaced daily versus weekly.
“We don’t know yet what the patches are going to be capable of,” Buse said. “In an ideal world, it’d be one patch a day or one patch a week. It’s going to take a while before we figure out what’s really possible.”





