Can You Measure Quality of Life?

First in a Series
In describing how best to care for a person who has diabetes, the Introduction to the 2017 Edition of the American Diabetes Association’s Standards of Medical Care says this:
Individual circumstances … above all, patients’ values and preferences, must be considered and may lead to different targets and strategies.
In 2016, when ADA presented a symposium under the banner Beyond A1C—Why Quality of Life Matters at the Annual Scientific Sessions in New Orleans, Dr. Lawrence Fisher told his audience that merely improving glycemic control was too limited a measure: “Patient quality of life can be a better predictor of mortality and morbidity than some biologic measures,” he said.
Dr. Fisher has been studying this idea for a long time, as a clinical psychologist, a professor at the University of California at San Francisco, and a clinical trial investigator. When he was a panelist at the 2016 ADA Scientific Sessions, he was talking about the ways that diabetes care clinical trials were designed, and how difficult it is to include a yardstick in a trial that will show how the patient’s life has been made better overall by following a course of treatment. He, and others, Dr. Mark Peyrot, for example, a sociologist who consults for pharmaceutical developer Novo Nordisk, have helped build a body of knowledge as to how people rate their own successes living with diabetes. Most of what has been learned has come from people who have answered questionnaires and surveys and been interviewed by their clinicians.
But that method has its limits. Richard Wood, chief executive officer at dQ&A, a company that specializes in market research for the diabetes care industry, believes that “eighteen minutes is about as much as a survey responder can take.” During a presentation on mental health and the need to “see beyond A1C” at the annual American Association of Diabetes Educators conference last month, he described results of 3,000 on-line surveys his company conducted during the summer of 2016 with people who have diabetes. Only a quarter of people with T2D taking oral medications, when they responded without any prompting to a general question about whether their health was better or worse than in the previous year, answered by reporting change in A1c. Weight gain or loss, success in following diets and exercise programs, and the costs of their medications and adequacy of insurance coverage were factors more people with T2D thought first about, along with daily burdens which they felt had been thrust upon them.
The odds of a life-shortening or disabling condition coming on have been thoroughly calculated over many years for people who have T2D. But there’ isn’t a column showing how hard it is for people to keep up the motivation to overcome those odds.
An article entitled “Type 2 Diabetes and Quality of Life” published in April of this year in the World Journal of Diabetes mentions that 1.95 million articles have been written on how diabetes erodes quality of life, more than have been written on cardiovascular, kidney, vision, limb loss, or neuropathic complications, or on the correlation between diabetes and emotional stress. Two overwhelming truths have emerged from all this research, even if it is difficult to measure them precisely:
- First, it’s not the blood glucose or the A1c numbers that create anxiety any near as much as the prospect of developing heart disease or having a stroke, or losing eyesight or the ability to walk
- Second, as with any chronic health condition, if there’s diminished hope of finding a path to being relieved of it, there’s no strong motivation to steadily pursue a health-promoting way of life
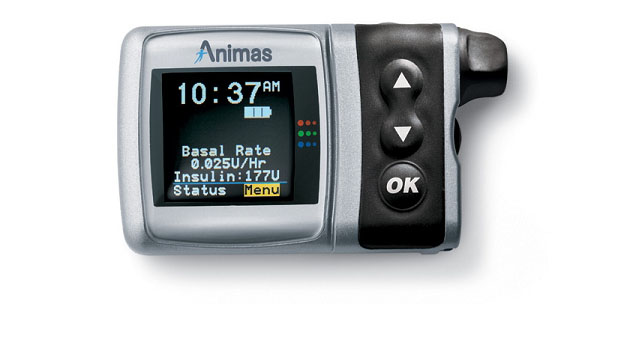
It’s possible to gauge that loss of motivation by looking at statistics, such as the Centers for Disease Control data on non-adherence to Type 2 medications, and finding the rates at which patients delay or abandon refilling prescriptions. The CDC estimates that 45% or more of Americans with T2D fall out of compliance with their oral or injected med schedules within a year of first being prescribed. When Novo Nordisk looked at utilization of its liraglutide GLP-1 drug in Europe in 2013, it found that only 60% of users followed their therapy through a 12-month period without a gap or without stopping entirely. Other surveys and estimates have uncovered that rates of adherence vary from medication to medication, and are materially affected by the inconvenience or complexity involved in proper self-administration.
Adam Brown, Mr. Woods’s co-presenter at the ADEA conference, and senior editor at diaTribe, estimated that fewer than a third of people who have diabetes feel that they are successful meeting their goals. The remark I’ve used to introduce this series – real life not being a randomized control trial – is his, made at the ADEA conference. His book Bright Spots & Landmines published in May 2017 devotes an entire chapter to cultivating a mindset for overcoming the daily burden of maintaining diabetic health — in other words, for maintaining one’s quality of life. In Chapter 2, Mr. Brown mentions that when he was diagnosed his blood glucose “numbers did feel like a grade, which drove me to check less often, and in turn, spend less time in range.” He endorses a recommendation from the Behavioral Diabetes Institute to write “It’s just a number” on a sticky note and keep it with your meter.
None of this, of course, makes it reasonable to downplay the need to keep track of blood sugar. The #beyondA1c movement that has gathered steam since the 2016 ADA Scientific Sessions, and that diaTribe reported on in July 2017, is not an instead of A1c movement. No responsible diabetes clinician would advocate abandoning measurement of A1c or BGL, or body mass, or blood pressure, or kidney function. Think about how your doctor measures the effectiveness of your medication, your diet, your daily care routine, when you go in for your checkup. And think about the information that comes from the manufacturers of your diabetes meds, and about how their effectiveness has been measured in the clinical performed during their development. The measure that’s always been accepted, all around the world, is lowering A1c and then keeping near that ideal number 7.
We all know why, don’t we? It’s because all roads beginning at loss of glycemic control lead to cardiovascular and kidney disease, blindness, and limb loss. Research is turning up links between dietary sugar and cancer and onset of age-related dementia. Maintaining quality of life is, after all, the central point.
In the next instalment we’ll look at the particular needs of seniors, and point to some strategies doctors often follow to ease the frustrations their aging patients face as they live with diabetes.
Adam Brown’s book Bright Spots & Landmines is available at Amazon and Barnes and Noble.
Want more news on Type 2 diabetes? Subscribe to our newsletter here.