COPD and Type 2 Diabetes
Rapidly growing worldwide diseases with high mortality and complex interactions with each other and with obesity

We spoke with Chaitanya Mamillapalli, MD, MRCP, FAPCR, Endocrinologist (bio) with the Springfield Clinic a 400 physician multi-specialty organization with more than 25 locations in downstate Illinois. Dr. Mamillapalli is the lead author of a review article on COPD and Type 2 Diabetes (source).
Why is the rate of COPD increasing?
“The rate of COPD is increasing worldwide due to smoking and an aging population. Systemic inflammation from pollution, dust/fumes, obesity, hypoxia and use of corticosteroids is also a factor in the growth of COPD.
Between 1980 and 2014, the rate of death from chronic respiratory diseases, such as COPD, increased by nearly 30 percent overall in the US. In 2015, 6.7 percent of all deaths were due to chronic respiratory diseases, which were the fifth leading cause of death
Key COPD Facts
The Global Burden of Disease Study reports 251 million cases of COPD globally in 2016 and the disease accounts for 5% of all deaths globally.
More than 90% of COPD deaths occur in low and middle-income countries.
The primary cause of COPD is exposure to tobacco smoke (either active smoking or secondhand smoke).
Other risk factors include:
- Indoor air pollution (such as solid fuel used for cooking and heating)
- Outdoor air pollution
- Occupational dust and chemicals (such as vapors, irritants, and fumes)
- Frequent lower respiratory infections during childhood.
- Some cases of COPD are due to long-term asthma.
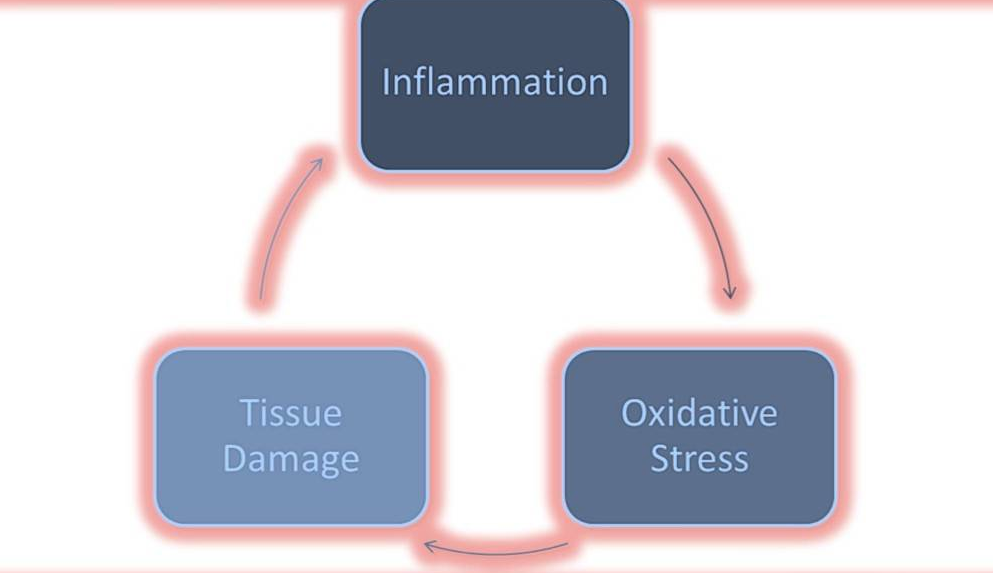
Chronic inflammation is a root cause
Chronic systemic inflammation is one of the common denominators between COPD and T2D.
- COPD is associated with chronic Broncho alveolar inflammation as well as systemic inflammation in response to noxious particles or gases, primarily those in tobacco smoke.
- Numerous studies have shown that low-grade chronic inflammation is part of the insulin resistance syndrome and is associated with the development of T2D.
How are these diseases related?
Epidemiological studies have found that T2D is more frequent in COPD patients and likely to affect their prognosis.
Findings from the Taiwan Longitudinal Health Insurance Database between 2000 and 2013
- At the time of COPD diagnosis, 16% of the patients presented with pre-existing T2D
- 19% of those without pre-existing DM developed incident DM within 10 years of diagnosis of COPD
- Both pre-existing and incident T2D were associated with an increased risk of all-cause mortality in COPD patients.
- Patients with COPD have a greater risk of T2D compared with control subjects
In a Swedish prospective population-based study of middle-aged Caucasian men, poor vital capacity predicted new-onset T2D.
If someone has diabetes, then hyperglycemia has been shown to be associated with reduced lung function, and an increase in the risk of COPD.
Obesity as a link between COPD and Diabetes?
Obesity is an overlapping risk factor for both COPD and T2D because obesity stresses all organs.
Obesity is one of the most important risk factors for T2D, in the development of insulin resistance and disease progression
- A Canadian national health survey stated that the prevalence of obesity was significantly higher in patients with COPD (24.6%) compared to patients without (17.1%).
- Another study in the US, conducted on early COPD patients noted that 54% of COPD subjects had a BMI > 30, compared to 20-24% prevalence in the normal population.
Obesity can cause both pulmonary and systemic inflammation by producing excessive inflammatory cytokines such as tumor necrosis factor Alfa (TNF-α) and interleukin-6 (IL-6), which may contribute to vascular and pulmonary damage
Role of oxidative stress results in disease progression
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3499352/figure/F1/
Reactive oxygen species are chemicals containing oxygen with an extra electron. Oxidative stress results from these free radicals. These reactive chemical entities are short-lived species containing one or more unpaired electrons. The free radicals induce damage to cells by passing the unpaired electron resulting in oxidation of cell components and molecules (Bansal and Bilaspuri, 2011). Oxidative stress is a phenomenon of the loss of balance between the making of reactive oxygen species (free radicals) and antioxidant defenses causing tissue damage.
Glucose, oxidative stress and inflammation are inter-related, with reciprocal causation. As the only glucose-lowering hormone in the body, insulin therapy alleviates the detrimental effects of hyperglycemia through metabolic regulation, therefore hyperglycemia is pro-inflammatory whereas insulin is anti-inflammatory.
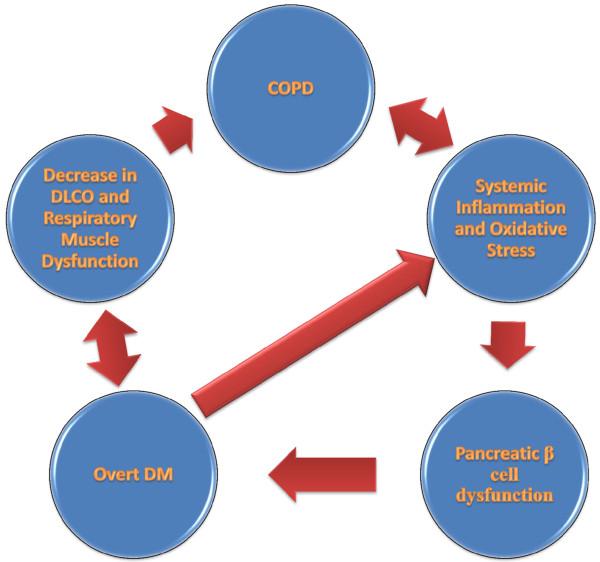
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3499352/figure/F4/
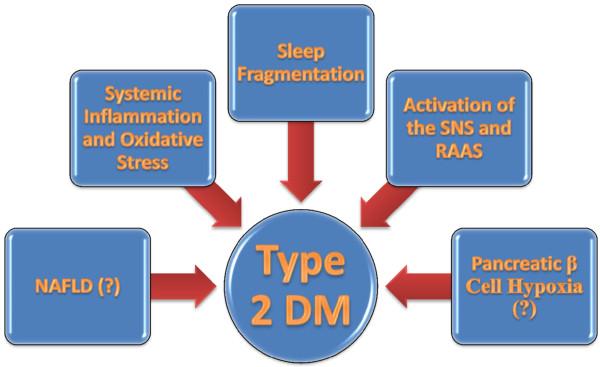
Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3499352/figure/F5/
CONCLUSION
There is overwhelming evidence of the association between the COPD and T2DM, and their intertwined pathologies.
- T2D patients should ask your endocrinologist to measure lung function to establish a baseline.
- People with COPD should ask their pulmonologist to screen them for T2Ds.
Timely treatment of COPD exacerbations, flu vaccination, and antibiotic use can result in the reduction of oxidative stress and systemic inflammation will reduce insulin resistance and optimize glucose control in T2DM patients. Achieving optimal glucose control is crucial in patients with coexistent T2DM and COPD, to prevent adverse outcomes in COPD patients and diabetic complications related to T2DM.





